All Departments
Emergency Cases
+91 86105 19191Opening Hours
- Tuesday - Saturday: 09:30 am - 07.30 pm

Varicose Veins
Varicose veins in leg are more common than previously thought. These are swollen veins, most frequently found in the legs but sometimes occurring on other parts of the body. Though they are not a serious condition they are often painful and inconvenient. They can also lead to other health issues if left untreated.
Ambulatory Phelbectomy is a surgical technique that does not leave scars after treatment.
When blood travels through your body, it relies upon valves in the veins. If any of these valves are damaged, blood does not move as efficiently, and it may collect in veins, causing them to swell. Valves may become damaged during extended periods without motion, either standing or sitting.
Although they can be painful and disfiguring, they are usually harmless. When inflamed, they become tender to touch and can hinder circulation to the point of causing swollen ankles, itchy skin, and aching in the affected limb.
Get rid of Varicose Veins by Endovenous Laser Ablation Technique
Besides a surface network of veins, your legs have an interior, or deep, venous network. On rare occasions, an interior leg vein becomes varicose. Such deep varicose veins are usually not visible, but they can cause swelling or aching throughout the leg and maybe sites where blood clots can form.
Abnormally dilated veins that appear on the legs are a common problem, affecting 30-50% of the population during their lifetime. They can affect both men and women and are more commonly seen in people with strong family history and may worsen with occupations that require prolonged standing, or even with pregnancy.
Presentations can range from those that are noticed incidentally to those causing significant symptoms. These are dilated superficial veins that are commonly seen in the legs. There are three types of varicose veins, which are usually seen in combination.
What Causes Varicose Veins?
When the walls of veins weaken, varicose veins grow. As the vein’s blood pressure rises, the weakened walls allow the vein to expand. The valves in the vein can’t function as well as they should as the vein expands. The vein swells, bulges, and twists as sluggish blood back up or pools in it.
Bulging, cord-like, distorted veins that are dark blue, red, or purple are apparent to the naked eye as varicose vein symptoms. Varicose veins can appear on the feet and legs, and they can also appear on the forehead. These veins can cause the surrounding skin to become extremely sensitive and tender, itchy, and cause aches in the limbs if they become inflamed.
- Hormones
- Family history of varicose veins
- The aging process
- Excess weight
- Muscle cramps in legs
- Swelling of feet or limbs
- Prolonged Standing over time
- Pregnancy
- Stretched skin taut over Varicose veins, if it has progressed or left untreated.
Sign & Symptoms :
- Aching & heaviness in legs
- Telangiectasia in the affected leg (also known as Spider Vein)
- Swollen Ankles
- Skin discoloration near the affected veins
- Redness, dryness, and itchiness of areas of skin
- Burning or Inflammatory sensations
- Abnormal bleeding or prolonged healing time for injuries in the affected area
- Muscle cramps while making sudden movements such as standing
Vein Problems Related to Varicose Veins
A number of vein problems are related to varicose veins, such as telangiectasias (tel-AN-juh-ek-TA-ze-uhs), spider veins, varicoceles (VAR-i-ko-seals), and other vein problems.
Telangiectasias
Telangiectasias are small clusters of blood vessels. They’re usually found on the upper body, including the face.
These blood vessels appear red. They may form during pregnancy and often are found in people who have certain genetic disorders, viral infections, or other medical conditions, such as liver disease.
Because telangiectasias can be a sign of a more serious condition, see your doctor if you think you have them.
Spider Veins
Spider veins are a smaller version of varicose veins and a less serious type of telangiectasias. Spider veins involve the capillaries, the smallest blood vessels in the body.
Spider veins often show up on the legs and face. They usually look like a spider web or tree branch and can be red or blue. They usually aren’t a medical concern.
Varicoceles
Varicoceles are varicose veins in the scrotum (the skin over the testicles). Varicoceles may be linked to male infertility. If you think you have varicoceles, see your doctor.
Other Related Vein Problems
Other types of varicose veins include venous lakes, reticular veins, and hemorrhoids. Venous lakes are varicose veins that appear on the face and neck.
Reticular veins are flat blue veins often seen behind the knees. Hemorrhoids are varicose veins in and around the anus.
Causes
Weak or damaged valves in the veins can cause varicose veins. After your arteries deliver oxygen-rich blood to your body, your veins return the blood to your heart. The veins in your legs must work against gravity to do this.
One-way valves inside the veins open to let blood flow through and then shut to keep blood from flowing backward. If the valves are weak or damaged, blood can back up and pool in your veins. This causes the veins to swell.
Weak valves may be due to weak vein walls. When the walls of the veins are weak, they lose their normal elasticity and become like an overstretched rubber band. This makes the walls of the veins longer and wider, and causes the flaps of the valves to separate.
When the valve flaps separate, blood can flow backward through the valves. The backflow of blood fills the veins and stretches the walls even more. As a result, the veins get bigger, swell, and often get twisted as they try to squeeze into their normal space. These are varicose veins.
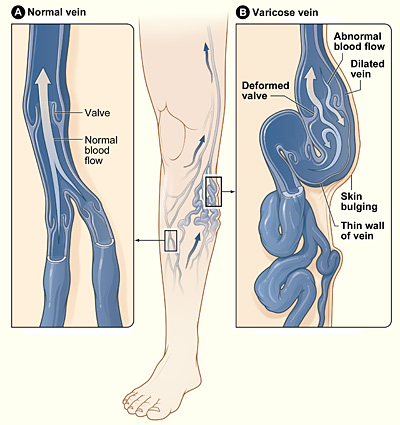
Normal Vein and Varicose Vein
The illustration shows how a varicose vein forms in a leg. Figure A shows a normal vein with a working valve and normal blood flow. Figure B shows a varicose vein with a deformed valve, abnormal blood flow, and thin, stretched walls. The middle image shows where varicose veins might appear in a leg.
You may be at higher risk for weak vein walls due to increasing age or a family history of varicose veins. You may also be at higher risk if you have increased pressure in your veins due to overweight or obesity, or pregnancy.
Risk Factors
A number of factors may increase your risk for varicose veins, including family history, age, gender, pregnancy, overweight or obesity, and lack of movement.
Family History
Having family members who have varicose veins may raise your risk for the condition. About half of all people who have varicose veins have a family history of them.
Age
Getting older may put you at higher risk for varicose veins. The normal wear and tear of aging may cause the valves in your veins to weaken and not work as well.
Gender
Women tend to get varicose veins more often than men. Hormonal changes that occur during puberty, pregnancy, menopause, or with the use of birth control pills may raise a woman’s chances of getting varicose veins.
Pregnancy
During pregnancy, the growing fetus puts pressure on the veins in the legs. Varicose veins that occur during pregnancy usually get better within 3 to 12 months of delivery.
Overweight or Obesity
Being overweight or obese can put extra pressure on your veins. This can lead to varicose veins.
Lack of Movement
Standing or sitting for a long time, especially with your legs bent or crossed, may raise your risk for varicose veins. This is because staying in one position for a long time may force your veins to work harder to pump blood to your heart.
Signs and Symptoms
The signs and symptoms of varicose veins include:
- Large veins that you can see on your skin.
- Mild swelling of your ankles and feet.
- Painful, achy, or “heavy” legs.
- Throbbing or cramping in your legs.
- Itchy legs, especially on the lower leg and ankle. This is sometimes incorrectly diagnosed as dry skin.
- Discolored skin in the area around the varicose vein.
Signs of telangiectasias are red clusters of veins that you can see on your skin. They’re usually found on the upper body, including the face. Signs of spider veins are red or blue veins in a web pattern that often show up on the legs and face.
See your doctor if you have these signs and symptoms. They also may be signs of other, sometimes more serious conditions.
Complications
Sometimes varicose veins can lead to dermatitis (der-ma-TI-tis), an itchy rash. If you have varicose veins in your legs, dermatitis may affect your lower leg or ankle. Dermatitis can cause bleeding or skin ulcers if the skin is scratched or irritated.
Varicose veins may also lead to a condition called superficial thrombophlebitis (THROM-bo-fleh-BI-tis). Thrombophlebitis is a blood clot in a vein. Superficial thrombophlebitis means that the blood clot occurs in a vein close to the surface of the skin. This type of blood clot may cause pain and other problems in the affected area.
Diagnosis
Doctors often diagnose varicose veins based on a physical exam alone. Sometimes tests or procedures are done to find out the extent of the problem and to rule out other disorders.
Specialists Involved
If you have varicose veins, you may see a vascular medicine specialist or vascular surgeon. These are doctors who specialize in blood vessel conditions. You also may see a dermatologist. This is a doctor who specializes in skin conditions.
Physical Exam
To check for varicose veins in your legs, your doctor will look at your legs while you’re standing or sitting with your legs dangling. He or she may ask you about your signs and symptoms, including any pain you’re having.
Diagnostic Tests and Procedures
Doppler Ultrasound
Your doctor may recommend a Doppler ultrasound to check blood flow in your veins and to look for blood clots. A Doppler ultrasound uses sound waves to create pictures of structures in your body.
During this test, a handheld device will be placed on your body and passed back and forth over the affected area. A computer will convert the sound waves into a picture of the blood flow in your arteries and veins.
Angiogram
Although rare, your doctor may order an angiogram to get a more detailed look at the blood flow through your blood vessels. For this procedure, dye is injected into your veins. The dye outlines your veins on x-ray images.
An angiogram can help your doctor confirm whether you have varicose veins or another problem.
Treatment Overview
Varicose veins are treated with lifestyle changes and medical procedures. The goals of treatment are to relieve symptoms, prevent complications, and improve appearance.
If your varicose veins cause any minor symptoms, your doctor may suggest simply making lifestyle changes. If your symptoms are more severe, your doctor may recommend one or more medical procedures. For example, you may need a medical procedure if you have significant pain, blood clots, or skin disorders as a result of your varicose veins.
Some people who have varicose veins choose to have procedures to improve the appearance of their varicose veins.
Although treatment can help existing varicose veins, it can’t keep new varicose veins from forming.
Lifestyle Changes
Lifestyle changes are often the first treatment for varicose veins. These changes can prevent varicose veins from getting worse, reduce pain, and delay other varicose veins from forming. Lifestyle changes include the following:
- Avoid standing or sitting for long periods without taking a break. When sitting, avoid crossing your legs. Raise your legs when sitting, resting, or sleeping. When you can, raise your legs above the level of your heart.
- Do physical activities to get your legs moving and improve muscle tone. This helps blood move through your veins.
- If you’re overweight or obese, lose weight. This will improve blood flow and ease the pressure on your veins.
- Avoid wearing tight clothes, especially those that are tight around your waist, groin (upper thighs), and legs. Tight clothes can make varicose veins worse.
- Avoid wearing high heels for long periods. Lower heeled shoes can help tone your calf muscles. Toned muscles help blood move through the veins.
Your doctor may recommend compression stockings. These stockings create gentle pressure up the leg. This pressure keeps blood from pooling and decreases swelling in the legs.
There are three types of compression stockings. One type is support pantyhose – these offer the least amount of pressure. A second type is over-the-counter compression hose, which give a little more pressure than support pantyhose. Over-the-counter compression hose are sold in medical supply stores and pharmacies.
Prescription-strength compression hose are the third type of compression stockings. These stockings offer the greatest amount of pressure, and are also sold in medical supply stores and pharmacies. However, you will need to be fitted for them in the store by a specially trained person.
Procedures & Surgical Interventions
Medical procedures are done either to remove varicose veins or to close them. Removing or closing varicose veins usually doesn’t cause problems with blood flow because the blood starts moving through other veins.
You may be treated with one or more of the procedures listed below. Common side effects right after most of these procedures include bruising, swelling, skin discoloration, and slight pain.
The side effects are most severe with vein stripping and ligation (li-GA-shun). Although rare, this procedure can cause severe pain, infection, blood clots, and scarring.
Sclerotherapy
Sclerotherapy (SKLER-o-ther-a-pe) uses a liquid chemical to close off a varicose vein. The chemical is injected into the vein to cause irritation and scarring inside the vein. The irritation and scarring cause the vein to close off, and it fades away.
This procedure is often used to treat smaller varicose veins and spider veins. It can be done in your doctor’s office, while you stand. You may need several treatments to completely close off a vein.
Treatments are typically done every 4 to 6 weeks. Following treatments, your legs will be wrapped in elastic bandaging to help healing and decrease swelling.
Microsclerotherapy
Microsclerotherapy (MI-kro-SKLER-o-ther-a-pe) is used to treat spider veins and other very small varicose veins. A small amount of liquid chemical is injected into a vein using a very fine needle. The chemical scars the inner lining of the vein, causing it to close off.
Laser Surgery
This procedure applies light energy from a laser onto a varicose vein. The laser light makes the vein fade away. Laser surgery is mostly used to treat smaller varicose veins. No cutting or injection of chemicals is involved.
Endovenous Ablation Therapy
Endovenous ablation (ab-LA-shun) therapy uses lasers or radiowaves to create heat to close off a varicose vein. Your doctor makes a tiny cut in your skin near the varicose vein. He or she then inserts a small tube called a catheter into the vein. A device at the tip of the tube heats up the inside of the vein and closes it off.
You will be awake during this procedure, but your doctor will numb the area around the vein. You can usually go home the same day as the procedure.
Endoscopic Vein Surgery
For endoscopic (en-do-SKOP-ik) vein surgery, your doctor will make a small cut in your skin near a varicose vein. He or she then uses a tiny camera at the end of a thin tube to move through the vein. A surgical device at the end of the camera is used to close the vein. Endoscopic vein surgery is usually only used in severe cases when varicose veins are causing skin ulcers. After the procedure, you can usually return to your normal activities within a few weeks.
Ambulatory Phlebectomy
For ambulatory phlebectomy (fle-BEK-to-me), your doctor will make small cuts in your skin to remove small varicose veins. This procedure is usually done to remove the varicose veins closest to the surface of your skin. You will be awake during the procedure, but your doctor will numb the area around the vein. Usually, you can go home the same day that the procedure is done.
Vein Stripping and Ligation
Vein stripping and ligation is typically only performed for severe cases of varicose veins. The procedure involves tying shut and removing the veins through small cuts in your skin. You will be given medicine to temporarily put you to sleep so you don’t feel any pain during the procedure. Vein stripping and ligation is usually done as an outpatient procedure. The recovery time from the procedure is about 1 to 4 weeks.
Limiting the Effects of Varicose Veins
You can’t prevent varicose veins from forming. However, you can prevent the ones you have from getting worse. You can also take steps to delay other varicose veins from forming:
- Avoid standing or sitting for long periods without taking a break.
- When sitting, avoid crossing your legs. Raise your legs when sitting, resting, or sleeping. When you can, raise your legs above the level of your heart.
- Do physical activities to get your legs moving and improve muscle tone. This helps blood move through your veins.
- If you’re overweight or obese, lose weight. This will improve blood flow and ease the pressure on your veins.
- Avoid wearing tight clothes, especially those that are tight around your waist, groin (upper thighs), and legs. Tight clothes can make varicose veins worse.
- Avoid wearing high heels for long periods. Lower heeled shoes can help tone your calf muscles. Toned muscles help blood move through the veins.
- Wear compression stockings if your doctor advises you to. These stockings create gentle pressure up the leg. This pressure keeps blood from pooling in the veins and decreases swelling in the legs.